DisAbility Etiquette (Part ONE)
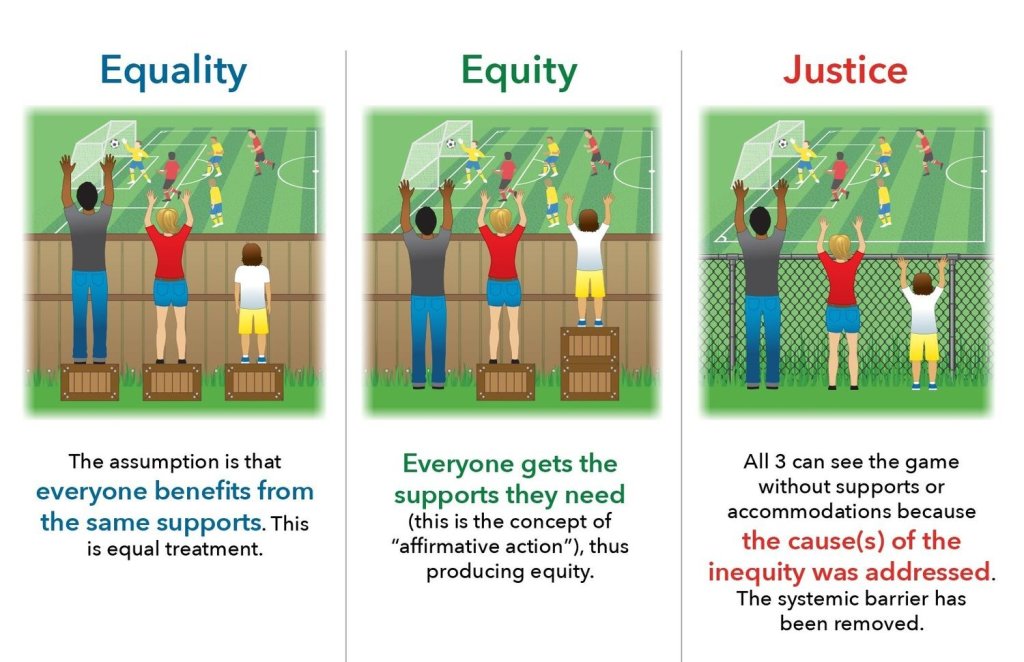
You cannot know how long I struggled with what to TITLE this piece! Having recently left a nearly 3-decades-long career in teaching (Psychology and ASL), I know how preoccupied folks are with being “inclusive” and equitable. Some even fully embrace being <GASP> WOKE. Folks who do not identify with any marginalized person group have shared with me (at least in the field of education and higher learning) that workshops, required certifications, and mandatory inclusive components more and more feel like “hoops to jump through”.
I can tell you that as a person with disabilities, the last thing I want abled people to feel about inclusive practices is relief at having a checkmark on their HR records. I love the way Emily Ladau (2021) simplifies best practices with an easy to incorporate “rule” in interacting with those who are differently-abled. “The Golden Rule” is simple and easy to live out with true authenticity. Treat others in the same way you would want to be treated. “You don’t need to start overthinking everything you say or do. That just makes things weird. Disability etiquette isn’t about tiptoeing around us and treating us like strange, delicate flowers (in fact, that’s pretty ableist in and of itself.) It’s about treating us like full and equal human beings” (Ladau, 2021, p. 89).
I truly believe (most) people mean well. Sometimes well-meaning intentions go awry, however. Yesterday, my husband and I went out to eat at a restaurant. My husband knows not to linger and hover over me as my service dog, Finn, gets me from “point A” to “point B” safely. Besides, he needed to make a “pit stop” so I walked out alone. As I navigated the last section near the door, I passed a booth with a family who had young children in it. Having lived the majority of my life with profound hearing loss, I do speech read fairly well. I saw one of the dads say to those at the table, “there’s a dog coming with a disabled person… don’t look, don’t stare, DON’T STARE”. Two of the three children (with age-appropriate ability to fully comply), dived under the table with one screeching, “I’m not looking at the dog! I’m not looking at the woman!”
I tell you what, I was so cracked up I had to stop and lean against my cane for a second before giggling my way to the door. As I passed the booth one dad was doing a classic “face palm” while the other mouthed, “SORRY” as I hobbled by. When I got outside, I had to do a “cane lean” again as I seriously nearly fell over laughing. Those dads didn’t need to warn the kids about my coming by. Finn is gorgeous, smart, and talented. I don’t mind the “look at the dog!” comments. I know the dad’s comments were meant in respect, but please… just treat me like a normal person. I have bling on my cane, cochlear implant, and hearing aid. My dog is an 85-pound, solid Golden Retriever. I’m not invisible nor do I care to be. If someone says, “What a pretty dog” as I walk by, I simply smile and say, “Thank you! He’s amazing”. I don’t consider noticing something that is VERY noticeable as being rude.

Photo description: Large Golden Retriever with royal blue service dog vest under a table at a restaurant.
To close out this two-part series on “DisAbility Etiquette”, I wanted to share some do’s and don’ts of two disabilities I have. [CHALLENGE: If you have other disabilities and would like to write for “Hearing Elmo” and share your own “do’s and don’ts” please contact me at denise.portis@gmail.com. I love having guest writers!]
In part two, I want to discuss some do’s and don’ts for people who use canes and service dogs for mobility challenges. In part one, I’d like to share some tips for interacting with people who have hearing loss. NOTE: I do “hear again” with a cochlear implant but these tips work for anyone with any degree of hearing loss, even those who are culturally Deaf.
DO:
- The Golden Rule (I won’t reiterate it again – smile)
- If you know someone has a hearing loss and you are hosting a workshop, meeting, or get-together, send an email or text to the person and ask what you could do to make the venue more accessible.
- Follow-up (especially work-related) meetings with an email to ask if they have any questions or missed any topics. (Careful with this one… don’t be condescending).
- If possible, secure captioning (transcription) for the meeting. Transcripts can be emailed to EVERYONE which only helps all present.
- Avoid small group activities where everyone is talking in small groups at the same time.
- If a person uses ASL, please provide an interpreter.
- Flicker the lights to bring the meeting to order. Yelling or wildly gesturing is rude.
- If there is a microphone present, USE IT. Don’t say, “my voice carries” or “I think everyone can hear me”.
- Insist others use a microphone from the audience, or repeat any questions asked.
- Write out on a white board or include a slide in a presentation if you are going to do any type of ice-breaker question, detailing what is being asked of participants.
DON’T
- Announce or otherwise bring attention to any one individual who may have trouble hearing.
- Raise your voice to a near shout.
- Turn your back to the audience to point to or gesture towards a screen or whiteboard.
- Talk to the interpreter of a culturally Deaf person, instead of talking to the person themselves.
- Play music or “theme songs” in between speakers.
- Use videos without captioning turned on
- Talk at the same time someone else is.
- Over enunciate speech
- Chew gum or have other items in your mouth when speaking.
- Hesitate to ask the person with disabilities if you are not sure how to proceed.
Ladau, E. (2021). Demystifying disability: What to know, what to say, and how to be an ally. New York: Ten Speed Press
L. Denise Portis, Ph.D.
© 2023 Personal Hearing Loss Journal












Much Love, Hearing Elmo. Much Love.